Today, data is an integral part of the healthcare landscape, providing insights that can make healthcare delivery more efficient and cost-effective. We spoke with Paul Bleicher, CEO of OptumLabs, about how the surge in the sources and volume of healthcare data is changing the industry.
What do you think will be the biggest innovations in healthcare tech in the next 10 years? Over the next 10 years, innovative new technologies will improve our ability to capture the patient experience from a variety of data sources and provide new approaches to analyze that data to provide accurate recommendations for a specific patient. Patient experience is a function of a variety of factors ranging from environment, to physiological measurements, to mental state, to opinion. This data will come from devices that we wear (activity monitors, etc.), devices that we use (smartphones, cars, scales, refrigerators), and sentiments we express through social media and other communications. Most importantly, it will be combined with data such as our medical record, to get a more complete, 360 degree view of our health, wellness, and wellbeing. Much of this type of data may be too detailed for consumption by any individual or health care provider. However, some of this data will help each of us, and our medical care team, better manage and understand our health and the decisions which influence it. In other cases, this type of data, aggregated for millions of patients, may be used to better understand the health of populations. In both cases it will provide insights that will greatly change the way care is delivered.
The explosion in availability of new kinds of patient data will be accompanied by a movement towards technologies leveraging prescriptive analytics to identify the best course of care. In the past, health care analytics have been descriptive (e.g. defining the characteristics of a population with a disease), explanatory (e.g. identifying the individual factors responsible for the disease), and even predictive (identifying and quantifying the risk of individual for developing a disease). These analytics are powerful, but can sometimes be overwhelming for an individual physician who is pressed to care for increasing numbers of patients with improved quality. The average physician is more interested in trustworthy prescriptive analytics which provide accurate recommendations for a specific patient. Cognitive computing and recommendation engines are two promising paths to such prescriptive analytics, but there will likely be many more new approaches to the analysis of individualized health care data.
What are the biggest challenges now and in the foreseeable future for the healthcare sector? The health care sector faces two related big challenges. One is the alignment of incentives and the other is information/data transparency in health care. In an ideal economic system with alignment of incentives, buyers of goods or services understand the cost of what they are buying, and understand the quality and value of what they are receiving, and how it will benefit them. The traditional buyer of health care services is an individual patient, but the entity paying for those services is typically an employer through a commercial payer, the Federal or State government. Historically, the insured patient, as well as the physician, typically had little exposure to the cost of health care because of a lack of transparency, and depended almost entirely upon their physician to advise them as to the need for and value of the care they were receiving. The payer, who was responsible for paying the bills of this care, had limited visibility into the patient’s care, again, due to a lack of transparency, and few tools to modify the physician’s behavior. This system, in place before the eras of capitation, HMO’s, and the current era of Accountable Care Organizations was untenable. It led to high costs, variable quality of care, and a complete lack of transparency for most of the participants. In most cases, the medical system acted in the patient’s best interest but excessive testing and treatment regularly occurred, often with the best of intentions.
Health care reform is attempting to address these issues. Increasingly, physicians participating in Accountable Care Organizations are taking financial risk for quality care, and patients are also taking financial risk through high deductible health plans. These are designed to begin the realignment of incentives needed to bring efficiency and high quality to health care.
In order to effectively realign the incentives, a second challenge needs to be overcome. Technology needs to be available to create transparency of information. Buyers of health care services need to know what they’re buying and its cost and quality, whereas clinicians need to understand the impact of their recommendations on cost for patients and their organization. This involves transparency of the cost effectiveness and quality of procedures, medications, and the delivery of health care services. With increasingly advanced analytic approaches, this data can be used by patients and providers to make better decisions, and for payers and employers to develop programs and guidance to encourage cost-effective and quality care. There is a lot being done in this area, and large companies like Optum are developing tools to enable patients, employers, and clinicians to understand gaps in care and opportunities for cost reduction and improved outcomes.
What is data’s role in healthcare tech and how do you see it influencing future innovations or sector growth? Data is central to health care technology. The interaction of a person with a piece of technology almost by definition today leads to the creation of a substantial amount of data. To ignore these data or to fail to collect them and use them in a comparative fashion is to miss one of the biggest opportunities for health system improvement. Whether collecting data about blood pressure, weight, interaction of the patient with their health care provider, physiological reaction of a patient to a medication – collecting that data and aggregating it into a database in a way that it can be compared and combined with other data and examined for trends, will allow us to better understand a patient’s interactions with the health system.
Data can be used both for understanding the individual patient with their consent, and with proper privacy protections, or it can be used in an anonymous, de-identified fashion to study and understand the health of populations of patients. By combining different sources of data that exist on a patient, a physician can assess and understand the impact of different activities and create predictions that not only provide better outcomes for patients, but also improve the cost and quality of their care. We have a big opportunity to use the kinds of machine learning technology developed by companies like Google and Facebook to instantaneously combine data on patient activities with other data from the same patient, or with data from other patients in order to diagnose an illness, identify the appropriate medication, course of treatment, and location of care. In this way, data is critical to health system innovation and improvement.
What are you most excited about that you’re working on now? We’re working with the National Quality Forum (NQF) on a handful of fascinating pilot projects to accelerate development of new health care performance measures. The NQF Measure Incubator is working in collaboration with OptumLabs to test how best to leverage big data resources and the expertise of some of our partners and other collaborators to develop novel performance measures.
Quality and performance measures have become an important part of health care today. They represent a meaningful way to improve access to care, quality and value of care and patient outcomes. Despite the widespread use of health care measures in the past two decades, many areas of health and health care still do not have enough or the right kinds of measures to provide the information needed to drive improvement. Additionally, many measures were developed at a time where electronic health records were less pervasive, thus limiting the data resources for development, and many also focused on process rather than outcomes. As a result, with the exception of the small but growing number of e-measures, most measures have been largely limited to the use of administrative claims data, or richer data from a few sites, and have been time consuming to develop.
We have a big opportunity now that there are claims and electronic medical record data available for millions of patients to create new measures that are patient-centered, outcome oriented, and for which results can be automatically extracted from electronic records. The opportunity to drive novel measurement discovery through measure creation, and to make measures more cost effective while reflecting the actual outcomes of care will be invaluable for identifying opportunities to improve health care value and patient care.
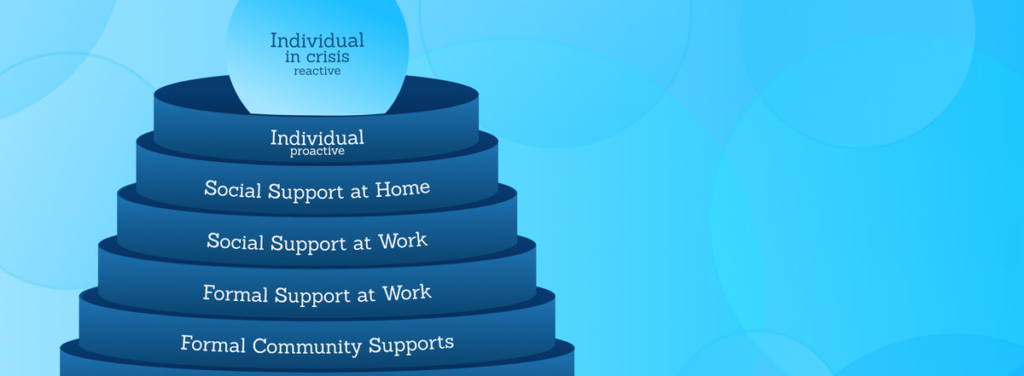
What opportunities are there for big data to bring payers and providers together? We’re seeing a convergence in OptumLabs of providers, payers and other health system stakeholders. Problems in health care tend not to be isolated to an individual group, and benefit from shared perspectives to solve them. For example, mental health has a dramatic effect on the cost, quality and outcomes of chronic disease. And that is a problem for the patient, provider, payer – everybody. What we’re doing at OptumLabs is bringing together diverse groups, including payers, providers, life science companies and consumer organizations who want to address these common problems and enabling them to collaboratively work together to solve them. Data is central to this effort. OptumLabs partners benefit from different perspectives and insights from data that can be applied to improve processes and outcomes. Also, because different organizations are working together, they have the opportunity to translate findings into new methods of care as a cooperative group rather than individually.